To jab or not to jab?
July 30
Vaccines have saved many lives and mark an important milestone in early childhood healthcare. But in a new trend, more people are refusing to get vaccinated, despite the wide availability of vaccines, writes Commonwealth Correspondent Omer Fayshal Pavel, 25, from Dhaka, Bangladesh.
Vaccines appeared as early as the year 1000, but it was only hundreds of years later that they were considered a major breakthrough in medicine.
In the 18th century, people lived in fear of a disease called the ‘speckled monster’. In Gloucestershire, England, a country doctor noticed that a dairymaid who had fresh lesions on her hands seemed to be fully protected from the disease. The doctor took pus from the lesions (caused by cowpox, a less deadly infection) and transferred it into a boy. Weeks later, the doctor then transferred the deadly ‘speckled monster’ into the boy, but he did not contract the disease. Edward Jenner was the physician credited with discovering the vaccine for the ‘speckled monster’ or smallpox in 1796.
Later, scientists like Louis Pasteur would develop other vaccines or antitoxins. Now, many organizations and pharmaceutical companies are working to develop vaccines for all manner of diseases. Many of these are recommended to be given to a child between birth and the age of six.
Vaccination is the administration of a vaccine to help the immune system develop protection from a disease. Vaccines contain a microorganism or virus in a weakened state, or proteins or toxins from the organism.
For centuries, vaccines have been considered the best way to protect populations against deadly epidemics such as smallpox, typhoid and tuberculosis. Most recently, vaccines have been used to prevent against deadly forms of flu, Ebola, and against the HPV virus, which is linked to cervical cancer.
However, vaccine hesitancy, a new trend where people refuse or are reluctant to get vaccinated despite the availability of vaccines, is on the rise. The World Health Organization (WHO) warns that this could reverse progress made in reducing vaccine-preventable diseases. In fact, vaccine hesitancy is considered among the top 10 threats to global health in 2019.
Measles has seen a 30% increase globally in cases reported, according to WHO. Although not all of these cases are due to vaccine hesitancy, some are. What is worrying is that countries that were close to eliminating the disease have seen a resurgence.
There are a number of reasons why people choose not to get vaccinated. Inconvenience in accessing vaccines, fears about vaccine safety or lack of confidence in the benefits of vaccines, and links between immunizations and autism (a behavioural disorder) are among these.
Religious and philosophical beliefs also play a role, as does misinformation that good hygiene eliminates the need for vaccination. Some of the physiological after-effects such as fever, rashes and pain put some off getting vaccinated.
WHO and other reputable agencies such as the US Centers for Disease Control and Prevention say vaccination is one of the most cost-effective ways to prevent infectious disease. Vaccines, WHO says, could prevent two to three million deaths a year. More than 1.5 million deaths could be avoided if global coverage of vaccinations improved.
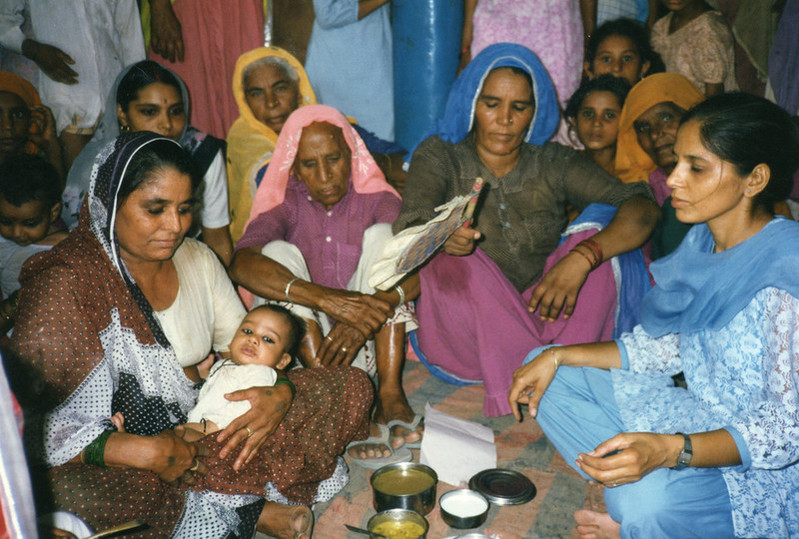
The Bangladesh government has initiated the Expanded Programme on Immunization (EPI) to ensure proper vaccination. EPI recommends five major vaccines that should be given to children within the first two years of life to protect against tuberculosis, diphtheria, Hepatitis B, whooping cough, tetanus, Haemophilus influenza-B, polio, measles and rubella.
In countries like Bangladesh, vaccine hesitancy must be addressed at grassroots level, particularly through health workers who are trusted advisors and influencers, especially in rural areas.
Public information and advocacy campaigns are important to get people to understand the benefits of vaccines and to bust some of the myths that currently cause people to avoid them.…………………………………………………………………………………………………………………
About me: I am a graduate and registered pharmacist from Bangladesh. My interest is working on drug development and clinical studies, with the motto of upholding the standard of public health. I have been involved in various national and multinational NGOs, especially in the health sector, and contributing health articles in national newspapers. I like to read about organic chemistry and molecular biology. I like traditional food, travelling and reading. I can speak Bangla, English, Hindi and French.
…………………………………………………………………………………………………………………
Opinions expressed in this article are those of the author and do not necessarily represent the views of the Commonwealth Youth Programme. Articles are published in a spirit of dialogue, respect and understanding. If you disagree, why not submit a response?
To learn more about becoming a Commonwealth Correspondent please visit: http://www.yourcommonwealth.org/submit-articles/






