“Our time with antibiotics is running out”
November 9 “Change can’t wait.Our time with antibiotics is running out,” is the message for World Antibiotic Awareness week from November 12-18.Omer Fayshal Pavel, 23, a Commonwealth Correspondent from Dhaka, Bangladesh, highlights the importance of antibiotics to our survival, arguing that its misuse puts us all at risk, he calls on both patients and physicians to urgently tackle this issue .
“Change can’t wait.Our time with antibiotics is running out,” is the message for World Antibiotic Awareness week from November 12-18.Omer Fayshal Pavel, 23, a Commonwealth Correspondent from Dhaka, Bangladesh, highlights the importance of antibiotics to our survival, arguing that its misuse puts us all at risk, he calls on both patients and physicians to urgently tackle this issue .
There are so many living things around us. But do we really think about those we cannot see? Known as microbes, some of them are so important that we can’t live without them. On the other hand, some are so life threatening that we depend on antibiotics to fight the diseases caused by them. Today however, the misuse and overuse of these substances, and poor infection management have contributed to rapid antibiotic resistance – a big challenge for our health systems and for human survival.
In 1928 Alexander Fleming, a Scottish biologist made a revolutionary discovery in medical science when he stumbled upon the antibiotic. He isolated Penicillium Notatum, a toxic substance from fungi, and surprisingly he found that though it was a toxin, it was not threatening to humans, but rather deadly to pathogens including certain bacteria that cause disease. Antibiotics kill bacteria and prevent their multiplication, and without antibiotics that work well, our very survival is in question.
Data from the World Health Organization (WHO) in 2012 shows that approximately 56 million people died that year. 32% of them died from infectious diseases namely malaria, tuberculosis and AIDS. Each year, these diseases cause millions of people of to fall ill and to die.
At one period in Bangladesh’s history, we were seriously affected by tuberculosis. Around 70,000 people per year died in the South Asian region because of the disease. It was not until 2006 that the successful use of antibiotics started to result in fewer deaths from tuberculosis.
Day by day however, antibiotics are losing their ability to fight these organisms. Even the once revolutionary penicillin has become less potent. This is a phenomenon known as antibiotic resistance.Instead of dying, microbes that cause infections are changing their make-up in response to antibiotic treatment, making it harder for people with these infections to get well, and infections that were once easily treatable are now more difficult and expensive to treat.
According to the WHO, “A growing list of infections – such as pneumonia, tuberculosis, blood poisoning, gonorrhoea, and food-borne diseases – are becoming harder, and sometimes impossible, to treat as antibiotics become less effective.”
In several cases, the antibiotic-resistant microbes have led to serious disability and even death.When one strain of a bacterium becomes resistant to antibiotic it can be spread through a cough, tears, urine, feces or any other biological product and make others ill. This makes antibiotic resistance an individual, community, national and global problem.
 When a patient doesn’t complete the dose of antibiotic prescribed, he or she is contributing to the problem of antibiotic resistance. When a doctor irrationally prescribes antibiotics, he or she is also contributing to antibiotic resistance.
When a patient doesn’t complete the dose of antibiotic prescribed, he or she is contributing to the problem of antibiotic resistance. When a doctor irrationally prescribes antibiotics, he or she is also contributing to antibiotic resistance.
Additionally, the rapid use of antibiotics in the agricultural sector is also contributing to the problem. While some antibiotics remain unchanged in crops and animal products, they can still act on the consumers’ body and contribute to antibiotic resistance.
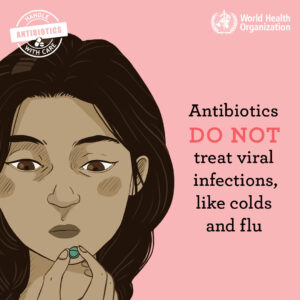
It is estimated that if the random use of antibiotics continues, without the development of new drugs, we may be facing an era in which people will increasingly die from illnesses like the flu.Globally, we urgently need to change the way we prescribe and use antibiotics.Even if new medicines are developed, without behaviour change, antibiotic resistance will remain a major threat.
Behaviour change must include actions to reduce the spread of infections through vaccination, hand washing, safer sex practice, and good hygiene.There are many initiatives to encourage the rational use of antibiotic like the World Health Assembly in May 2015 Global Action Plan on Antimicrobial Resistance. Resources are also available at the World Antibiotic Awareness Week website.
Whether its to treat meningitis or malaria, tuberculosis or HIV/AIDS, we need antibiotics that can restore our health and save lives.Without these antibiotics, our very survival is in question.
photo credit: https://pxhere.com/en/photo/566564 (license)
…………………………………………………………………………………………………………………
About me: I am a youth from Bangladesh, a country which is densely populated. The overpopulation has created issues that reduce the environmental and health status. As a result, different unexpected health challenges are affecting us. My ambition is to help us to overcome these problems by creating a network of youths and working as public health professional in the future.
I like to visit different places with different traditions and taste different foods. Right now I am a student of Pharmaceutical science and a health columnist for national newspapers.
…………………………………………………………………………………………………………………
Opinions expressed in this article are those of the author and do not necessarily represent the views of the Commonwealth Youth Programme. Articles are published in a spirit of dialogue, respect and understanding. If you disagree, why not submit a response?
To learn more about becoming a Commonwealth Correspondent please visit: http://www.yourcommonwealth.org/submit-articles/
…………………………………………………………………………………………………………………






